Research
Poster Abstract
2025 American Psychiatric Association Conference
The Reading, Television, Music, Meditation, Social-Interaction, Electronics (RTMMS-IE) Longitudinal Observational Correlation Outcomes Study of Patients Receiving Repetitive Transcranial Magnetic Stimulation (rTMS)
Authors: Y Pritham Raj, MD¹²; Nicholas Lindberg, MS².
1 Associate Professor, Depts. of Internal Medicine & Psychiatry, Oregon Health & Science University, Portland, OR, USA; Chief Medical Officer, Active Path Mental Health
2 Active Path Mental Health Research Group
Background
A standard course of left-sided high-frequency rTMS consists of 36 daily 20-minute sessions and is a well-established treatment for severe treatment-resistant depression (TRD). During each session, patients engage in a variety of self-selected activities, which can be broadly categorized as social or non-social. To date, we are not aware of any studies that have examined whether the type of in-session activity influences rTMS outcomes. We attempted to determine whether patients who engage in social activities during rTMS sessions have better outcomes.
Methods
This was a prospective observational correlation outcomes study of 107 consecutive consenting patients between 18 and 80 years old (67 female, 40 male) with a diagnosis of severe TRD without psychotic features who received at least 10 rTMS treatment sessions (mean 32.2 sessions) from November 2023 through May 2024 using either an H1-coil (n=39) or figure-8 coil (n=68). The primary outcome measure was change in Patient Health Questionnaire-9 (PHQ-9) score at the end of treatment stratified according to observed in-session activity as recorded by trained TMS technicians. There was a session-by-session assessment of whether there was social interaction with the TMS technician (or other support individual(s) in the room) or engagement in non-social activities such as reading, watching television, listening to music, meditation, or the use of personal electronics.
Results
To ensure the sample in the RTMSS-IE study was comparable to our previous, large (n=555) DONT H8 study (1), we conducted a two-sample t-test assuming equal variances between the two datasets. The t-test showed no significant variance between the samples (p=0.07), which also indicated that the methodology used in this study likely did not impact patient outcomes. The mean percent reduction in PHQ9 score for the cohort was 43.3 (sd=0.343). A Pearsons correlational analysis was then performed to examine the relationship between in-session activities (social and non-social) and reduction in PHQ-9 (and GAD-7) scores showing: PHQ-9/social activity (r=0.063, p=0.517), PHQ-9/non-social activity (r=-0.065, p=0.507), GAD-7/social activity (r=0.062, p=0.519), GAD-7/non-social activity (r= -0.063, p=0.527), all indicating no significant difference in outcomes between the groups. In a subgroup analysis, patients who spent >75% of sessions participating in social activity showed a 51% mean reduction in PHQ9 score compared to 38% for those spending > 75% in non-social activity (n=54, p=0.238, df=52, r=0.163).
Conclusions
The RTMMS-IE study suggests that choosing social or non-social activities during TMS treatment sessions does not correlate with depression outcomes. This suggests that the impact of rTMS is independent of self-selected patient activity during treatment, which is an important clinical finding. The subgroup analysis suggests that patients who spend more than 75% of their time in treatment engaged in social interaction may have better outcomes than those who spend more than 75% of their time in non-social interaction. Larger studies are needed to determine if such differences exist.
Conflict of Interest: None
Funding: No outside funding was obtained.
Disclosures: Dr. Raj is a lecturer for MedStudy.
Reference: 1. Raj YP, Lindberg N. Dual Observation Naturalistic TMS study comparing H1 and Figure-8 Coil outcomes (DONT H8). Brain Stimulation 2022;15(5):1322.
Poster RTMMS-IE
2025 American Psychiatric Association Conference

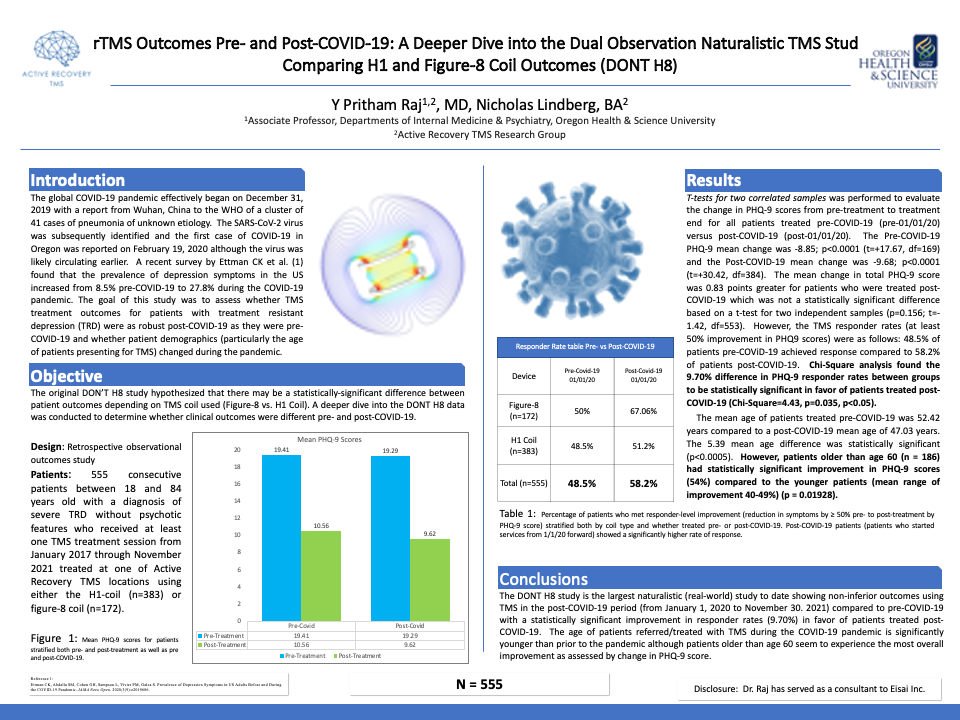
Poster #1 – DONT H8
2022 Clinical TMS Society Conference
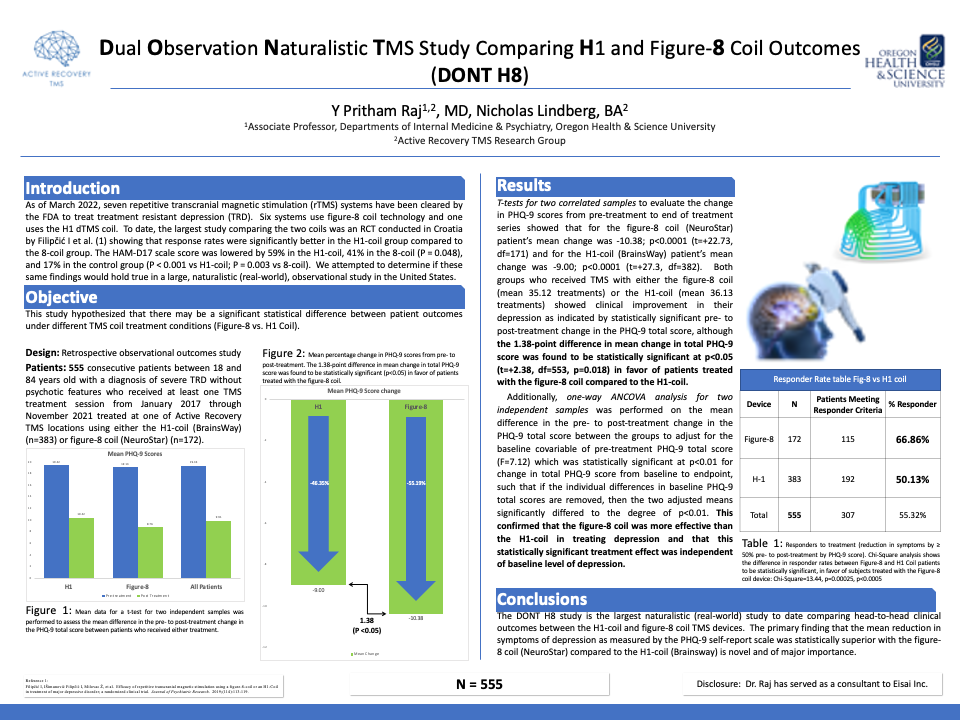
Poster #2 – DONT H8
2022 Clinical TMS Society Conference